Afex Incontinence Management System for Men
Our mission is to improve the quality of life and care for people around the world by developing and commercializing innovative male incontinence products and transformational technologies for healthcare. Since 2002, our mission-focused determination has guided us to develop patented and proprietary medical devices that offer significant benefits to patients and caregivers who use our incontinence products every day. Our current brands offer patients access to innovative daytime and nighttime incontinence products and technologies for management of incontinence, bladder leakage, and other urinary management needs.
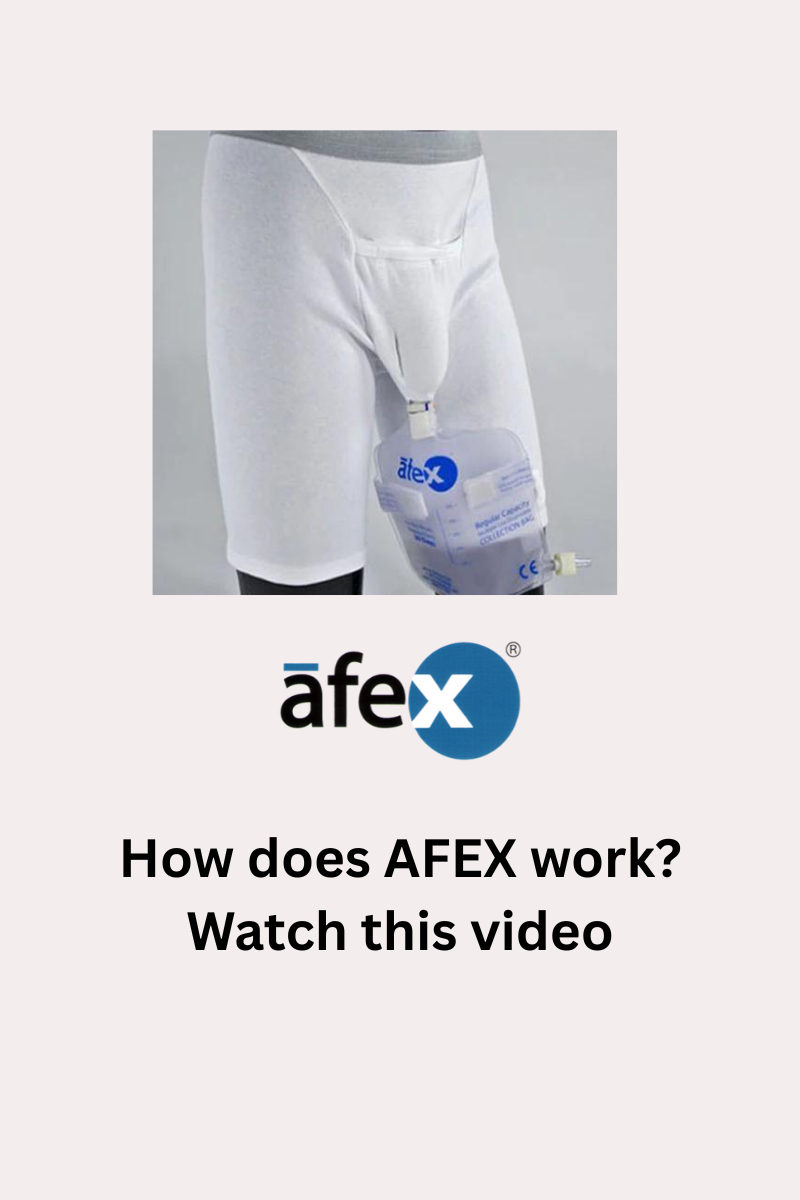
Afex® provides superior daytime protection with its patented receptacle and direct-connect collection bag. The receptacle and bag is discreetly supported by a comfortable, specially designed cotton brief or supporter. Patients who use our Afex® system enjoy the benefits of an innovative male incontinence product that effectively controls odor, leakage, and wetness often associated with other male incontinence products.
All Afex® Products are proudly Made in the USA









Afex Starter Kit with Sports Briefs for Active Daytime Use A100-SA-H
For active men without movement restrictions, the Afex Daytime kit offers excellent protection against mild to moderate urinary leakage. This day kit is a must-have for men who frequently need to use the bathroom. The Day Kit is seamlessly hidden and can be worn discreetly under your everyday pants!
The standard Afex® Active Starter kit contains everything you need to begin using Afex®. It includes:
- 1 full brief - sports active style
- 1 high style receptacle
- 1 standard 500 ml collection bag
- 1 cleaning container 4 oz bottle of liquid cleanser concentrate
Please specify your brief waist size. The high style receptacle is recommended for active and night use. Low style receptacle is generally recommended for more sedentary or mobility assisted use.
Free shipping on domestic orders over $100
Healthcare Provider Perspective
Prostate issues are a common cause of male incontinence symptoms. An enlarged prostate, known as Benign Prostate Hyperplasia (BPH), is more common among older men and BPH can cause varying levels and types of male incontinence. In the video below, Dr. Ryan Barnes from Virginia Urology in Richmond, Virginia talks about BPH, its symptoms, what causes it and how it is treated. Enlarged prostate or Benign Prostatic Hyperplasia (BPH) affects over 17 million men in the U.S. according to Virgina Urology. You can visit Virginia Urology at www.uro.com.
How to Use and Maintain Your Afex Male Incontinence System
The Importance of Managing Male Incontinence for Overall Health
Work Stress and Male Urinary Incontinence: Are They Connected?